Authors: Sonja Müller and Leo Lewis
Many regions across Europe are starting to develop and implement value-based care models.
Value in health and care is defined as patient outcomes (and sometimes experiences) in relation to the cost to deliver those outcomes. Value-based procurement therefore goes hand in hand with value-based care as purchasing decisions take into consideration how a product, solution, or service can best deliver the outcomes and experience of care being measured and reduce the total cost of care – rather than focusing exclusively on purchasing a specific product at the lowest possible price.
In our opinion, value-based innovation procurement can help foster more integrated, patient-centred care as it shifts the focus from traditional product buying to services and solutions delivering true value to the patient. Integrated care is an ongoing policy response across EU regions which aims to address inter-related financial, organisational, and person-centredness issues to provide sustainable health, social care, and support services.
Nevertheless, when it comes to incorporating the concept of integrated care into value-based care, we are still in relatively uncharted waters. This is what led us to participate in the European Wide Innovative Procurement of Health Innovation (EURIPHI) project, which had an integrated care workstream. Our work on the EURIPHI project underscored how value-based innovation procurement can incentivise all stakeholders – patients, health and care professionals, procurers, industry, and regional authorities/ payers – to collaborate on providing a personalised treatment program to achieve the best possible outcome while keeping costs in check.
We believe that significant progress has been made within the EURIPHI project, but we also recognise that some challenges remain. Below we share some experiences and insights from this project, using the stroke care pathway as an example.
Identifying Integrated Care Procurement Objectives
A main objective of the EURIPHI project’s integrated care arm was to increase understanding and organise the demand side around a small set of Integrated Care Procurement Objectives (ICPOs) to address identified integrated care service delivery shortcomings. In addition, we sought to assist EURIPHI partners and other European public procurers in the application of the most economic advantageous tender (MEAT) methodology to procurement. The goal is to address fragmentation in care services and enable better coordinated and more continuous care for people with health, social care, and support needs or any combination thereof.
The integrated care work commenced with a desktop research exercise to identify integrated care delivery shortcomings for five conditions:
- Stroke;
- Chronic obstructive pulmonary disease (COPD);
- Multimorbidity;
- Dementia; and
- Aortic stenosis.
For each of the topics, we identified care delivery issues along the end-to-end patient pathway, considering vertical care delivery shortcomings within each element of the patient pathways as well as horizontal care delivery shortcomings that span across all pathway elements and are important to facilitate an integrated and seamless transition between the different elements of the patient pathway. The example for the stroke pathway is presented below.
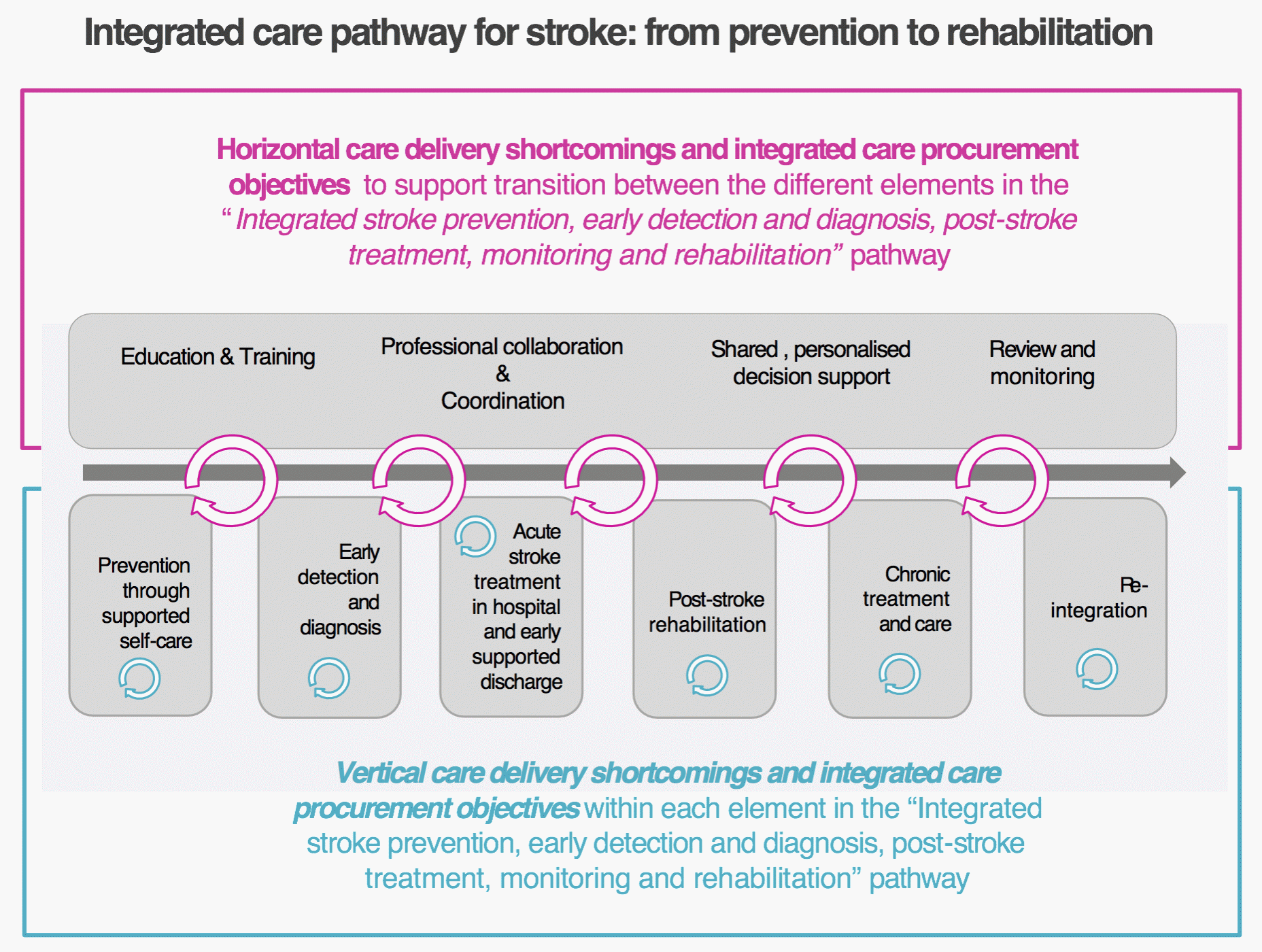
Stroke is a complicated, heterogeneous condition with acute onset but complex and enduring treatment and follow-up. Consequently, stroke care is complex and covers a whole spectrum of care including acute care, rehabilitation and long-term care with in-hospital, outpatient, and community-based care. Stroke care is thus by definition multidisciplinary, and the integration of care is of particular concern.1
For each pathway element, we analysed demand and supply side state-of-the-art, which resulted in the formulation of care delivery issues. Below are some of the issues we identified:
- Risk assessment online tools are limited to a single language domain and are not integrated even with local health records or professional platforms and records. Only pull media is used and there is no interface with health systems to draw risk parameters or to deliver assessment results back into the relevant systems.
- Socio-economic disparities exist. Across Europe, primary and secondary prevention strategies are not working well enough to control hypertension, which is one of the main controllable risk factors for stroke2. Existing racial disparities in stroke incidence highlight the importance of stroke prevention interventions aimed at minority groups3.
- There is a lack of bi-directional connectivity of devices. Where connectivity is available it is unidirectional, i.e., values can only be transferred out of the device. Any input, including adaptation to therapy parameters, needs to be manually set. There are innovative, medical grade devices, but these tend to be costly and therefore only suited to research use.
- Current treatment paradigms do not consider individual differences. Stroke care could be significantly improved by more personalised risk calculation and individualised therapeutic recommendations. Data sharing and infrastructure needs must be addressed, such as integrating highly heterogeneous multi-scale data sources, integrating ‘omics’ data into clinical care4, or integrating imaging data5.
- Deficits in communication and collaboration during the discharge planning process are common6. One big area of concern to patients and carers is the organisation of discharge from hospital as they move from being cared for by a team of professionals, to being at home and the responsibility of themselves and their carers7.
- Lack of rehabilitation is a big bottleneck in stroke treatment8. The demand for rehabilitation increases simultaneously with the rising number of strokes worldwide. Not enough information about ICT tools is promoted to facilitate the recovery process for stroke survivors.
Care delivery issues were then translated into ICPOs describing what an innovative solution would need to deliver to address one or more care delivery shortcoming(s). Highlights of the stroke ICPO include, among other things:
- Address lack of electronic care record data integration from technologies designed to motivate and educate people and enhance patient/care team interface.
- Address lack of integration of nutritional and physical activity information and advice.
- Link stroke risk assessment results with an interface for care practitioners to ensure that the identified person with high risk of stroke can be monitored and followed up.
- Address provision of bi-directional communication channels.
- Improve transition from hospital to home/community setting.
In total, 36 ICPOs for all five topics were included in a survey to elicit procurement priorities and feedback from the EURIPHI public procurement organisations (PPOs). Our analysis of survey responses resulted in 13 ICPOs going through to a survey widely distributed to other European regions and PPOs, the results of which produced a short-list of six ICPOs for consideration by the EURIPHI PPOs and Advisory Board members. We consolidated the six ICPOs into a final list of three, which went forward to an Open Market Consultation to determine whether there were innovative solutions available to address the care delivery shortcomings identified.
The ICPOs and associated care delivery shortcomings identified for the five conditions were not dissimilar, and this resulted in the final three ICPOs being described generically with specific examples of applicability for each condition. This maximised the opportunity to identify innovative solutions with broad integrated care reach rather than condition-specific and potentially provided a stronger business case for PPO investment.
Reflections and observations as we move forward
Coming into the EURIPHI project, we found that this was the first time some stakeholders had looked at value-based procurement from an integrated care perspective. As such, the value-based MEAT framework was largely focused on procurement initiatives relating to hospital interventions and very discrete aspects of an acute episode of care, with a start and an end point that could be quantified easily.
On the other hand, integrated care is a concept – a group of design principles that should be applied to deliver effective and efficient care across a continuum. Looking again at the stroke care pathway, rehabilitation starts in the receiving acute stroke specialist centre, but later the patient is discharged home or into a community setting, where the rehabilitation may be continued by, for instance, physiotherapists and occupational therapists employed by local authorities.
Particularly in the five health areas that we reviewed, care is being delivered across sectors (e.g., health, social care, and often support services). Thus, when considering procurement, the benefit often sits with an organisation that is further downstream, rather than the organisation initiating the procurement. This makes it unclear who would have the incentive to procure an integrated care solution and raises some complex questions:
- Who is the procurer of an innovative solution?
- Does that innovative solution span the whole of the pathway?
- Where are the benefits being realised, and for which stakeholders?
These questions led to very productive discussions with our EURIPHI partners who collaborated to modify the value-based procurement framework (MEAT) to reflect the different stakeholders’ perspectives in relation to integrated care where pathways and care cycles are part of a care continuum, particularly for people living with chronic conditions. Some ways in which we revised the framework included ensuring the language encompassed the health and care workforce rather than just health, the relevant original measures of value under the different dimensions reflected health and social where necessary, and new measures of value were developed to provide a comprehensive overview of innovative solutions from all stakeholder perspectives.
This experience has furnished us with new learning and tools that we can now take forward into other European projects. Likewise, the EURIPHI regions are keen to disseminate this work through international conferences and other suitable forums, with a view to moving the European health and care system towards a value-based approach to procurement as well as care delivery.
Please click here to view the fully referenced footnotes.
Sonja Müller (female) is senior researcher at empirica. She holds a degree in geography, urban development, and economic sociology from Bonn University. Since joining empirica in 2001, her main fields of work are in the area of digital solutions for integrated care, health & social care and independent living. Her expertise relates to requirements research & needs analysis, service process development, evaluation as well as cost-benefit-analysis and business model development. Through her work in projects such as VIGOUR , SmartCare and BeyondSilos she can base her work on a multitude of successfully concluded and ongoing implementation activities. Sonja is currently involved in the H2020 Coordination and Support action EURIPHI and in the project VIGOUR that is co-funded by the European Union’s Health Programme and designed to guide and support 15 care authorities across seven European countries in making progress towards the provision of sustainable models for care integration. She also works as an international expert in a project for DG REFORM “Supporting Integrated Service Provision Reform in Estonia” where her work focuses on care process pathway design. Since 2016 she is one of the co-ordinators of the EIP AHA B3 Action Group on “Integrated Care”. Her profile includes extensive publishing and conference activities, also encompassing organisation of small-scale workshops and large-scale conferences.
Leo Lewis, Director of Research & Development, International Foundation for Integrated Care. Leo has extensive experience of integrated care, digital health and care innovation through her role in leading a number of programmes and work packages focusing on chronic conditions management, disability, dementia and digital health whilst working for NHS Wales and over the last seven years with IFIC. Leo chairs the European Innovation Partnership on Active and Healthy Ageing, B3 Action Group on Integrated Care and Digital Solutions and is currently collaborating with the European Observatory on Health Systems and Policies on building a platform for evidence-based integrated care practices. As an experienced programme manager having working in academia, the NHS and Welsh Government leading eHealth, chronic conditions management service improvement and research projects, Leo was responsible for the development and testing of NHS Wales’ predictive risk modelling (Prism) tool. Through the building of strong relationships with stakeholders, Leo works with others to bring her knowledge, skills and expertise together to co-design new transformational change approaches for delivering integrated care solutions to meet the needs of different populations and is currently an international expert leading the care pathway redesign and care coordination work streams in a DG REFORM “Supporting Integrated Service Provision Reform in Estonia” project.




